Know the signs and act early
Body Image and Eating Disorders Awareness Week (BIEDAW) is a national week to raise awareness of body image concerns and eating disorders, celebrated annually in the first full week of September.
Eating disorders impact over 1 million Australians each year, and have one of the highest mortality rates of any mental illness. With only 1 in 10 Australians able to recognise the signs of an eating disorder, we urgently need people to familiarise themselves with common symptoms, particularly as presentations of eating disorders and demand for services continue to grow with the pandemic.
This BIEDAW, Butterfly will be joining our Eating Disorder Alliance Australia colleagues to raise awareness and encourage people to act early – because early intervention can have a marked difference on an eating disorder’s severity and duration.
From teachers, to friends, parents and healthcare professionals – everyone has a part to play in early intervention of eating disorders.
What is early intervention?
Early intervention refers to the identification of eating disorder symptoms and implementation of support and treatment for a person as soon as symptoms are recognised. This also relates to the early identification and response to re-emerging symptoms for someone who has recovered from an eating disorder. Its aim is to minimise the severity and duration of the disorder and to reduce its broader impacts.
“The longer disordered behaviours and negative thought patterns exist for an individual, the harder they are to break. They become a safety net and a maladaptive way of coping, so the fear of letting them go increases, making recovery incredibly long, difficult, and expensive.” – Grace, (she/her), 25, VIC, member of Butterfly’s lived experience network, The Butterfly Collective
Why is it important to Know The Signs and Act Early?
Eating disorder stereotypes, misconceptions and stigma sadly prevent many from seeking the help they deserve.
Many people struggle with symptoms for many years or even decades, with around 25% of people with an eating disorder experiencing a severe and enduring form of this mental illness. On average, eating disorder recovery can take up to six years.
With early detection and intervention, prospects of recovery are increased and high; it’s never advised to ‘watch and wait’.
If you’re worried or concerned about a loved one or someone you know, recognising the signs, acting early and knowing how to safely start the conversation is imperative.
“Early intervention is important in helping to break thought patterns and behaviours that become so ingrained over time. I am now in recovery but have been living with my eating disorder for over 20 years. Had I received some early intervention, these long-held patterns and beliefs may have been easier to accept and change.”
– Sally (she/her), 52, VIC, member of Butterfly’s lived experience network, The Butterfly Collective
How can people make early intervention possible?
Everyone’s experience of an eating disorder is unique and can present in a variety of ways. It’s not always easy to detect who may have an eating disorder – they come in all shapes and sizes and don’t have a “look”.
However, a range of behaviours and symptoms may be commonly observed in people experiencing eating disorders. These could include:
Physical warning signs
- Rapid weight loss or frequent weight changes
- Loss or disturbance of menstruation
- decreased libido
- Fainting or dizziness
- Feeling tired and not sleeping well
- Lethargy and low energy
- Signs of damage due to vomiting including swelling around the cheeks or jaw, calluses on knuckles, damage to teeth and bad breath
- Feeling cold most of the time, even in warm weather
Psychological warning signs
Psychological warning signs can be difficult to detect in anyone suffering from an eating disorder. They usually only come to light through changes in behaviour or through discussion and conversation.
- Preoccupation with eating, food, body shape and weight
- Feeling anxious and or irritable around meal times
- Feeling ‘out of control’ around food
- ‘Black and white’ thinking (e.g. rigid thoughts about food being ‘good’ or ‘bad’)
- A distorted body image
- Using food as a source of comfort (e.g. eating as a way to deal with boredom, stress or depression)
- Using food as self-punishment (e.g. refusing to eat due to depression, stress or other emotional reasons)
Behavioural warning signs
- Dieting behaviour (e.g. fasting, counting calories/kilojoules, avoiding food groups such as fats and carbohydrates)
- Eating in private and avoiding meals with other people
- Evidence of binge eating (e.g. disappearance and/or hoarding of food)
- Frequent trips to the bathroom during or shortly after meals
- Vomiting or using laxatives, enemas, appetite suppressants or diuretics
- Changes in clothing style (e.g. wearing baggy clothes)
- Compulsive or excessive exercising (e.g. exercising in bad weather, continuing to exercise when sick or injured, and experiencing distress if exercise is not possible)
- Changes in food preferences (e.g. claiming to dislike foods previously enjoyed, sudden preoccupation with ‘healthy eating’, or replacing meals with fluids)
- Obsessive rituals around food preparation and eating (e.g. eating very slowly, cutting food into very small pieces, insisting that meals are served at exactly the same time every day)
- Extreme sensitivity to comments about body shape, weight, eating and exercise habits
- Secretive behaviour around food (e.g. saying they have eaten when they haven’t, hiding uneaten food in their rooms)
While anyone can develop an eating disorder, there are certain populations who may be more at risk, and signs and symptoms may present differently. Find out more about who eating disorders affect.
Eating disorders and neurodivergence
Among all people with eating disorders, an estimated 30% is thought to be Autistic. People with ADHD have a 3- 6 times greater risk of developing an eating disorder. Eating disorder treatment is often designed for neurotypical people, and research demonstrates that current approaches are significantly less beneficial for Autistic women.
Eating Disorders Neurodiversity Australia (EDNA) is a not for profit, neurodivergent-led organisation whose board members have lived or living experience of an eating disorder. EDNA have created the below factsheet to explain how interoception influences the ways neurodivergent people experience body image issues and eating disorders.
Eating disorders and the LGBTQIA+ community
Homophobia, transphobia, gender dysphoria, discrimination, bullying, trauma, abuse and alienation from friends or family members can all result in high levels of emotional stress. Sometimes these issues, in addition to other risk factors, can contribute to the development of body image issues or an eating disorder.
LGBTQIA+ adults and adolescents experience greater incidence of eating disorders and disordered eating behaviours, have more severe ED symptoms, higher rates of trauma history and longer delays between diagnosis and treatment than their heterosexual, cisgender counterparts.
There’s no right or wrong way to approach someone with an eating disorder, and different approaches will work for different people at different times. It’s never advised to ‘watch and wait’ – If you or someone you know has concerns about disordered eating, it is important to seek help immediately.
How to start the conversation
Download our factsheet for tips and advice on how to approach someone you care about.
CONVERSATION STARTERS FOR EARLY INTERVNTION
Be curious and go gently. Ask open-ended questions, respond compassionately and non-judgmentally, and be patient. Know that you may sometimes be speaking to their eating disorder self – but that it’s distinct from their healthy self. Recognise that people may not know what kind of support they need from you, but that you can figure out what that might be together. – Jeanette (she/they), 23, VIC, member of Butterfly’s lived experience network, The Butterfly Collective
Get support
The first step to recovery from an eating disorder or body image issue is often seeing a health professional, such as your GP. Butterfly’s Referral Database can help you search for health professionals who are qualified in treating and support eating disorders.
You can also contact Butterfly’s National Helpline for confidential and free support for eating disorders and body image concerns. Our counsellors are available 7 days a week, 8am-midnight (AEST).
Call 1800 ED HOPE (1800 33 4673), chat online or email support@butterfly.org.au
Eating disorders are still vastly misunderstood, underestimated and undiagnosed; only one in 10 Australians can recognise the signs and symptoms of eating disorders, and less than one in four people with eating disorders will seek professional help.
Stigma and shame have been identified as key barriers in early intervention. To reduce this, there needs to be a shift in the attitudes and knowledge of the general community about eating disorders.
- One in four perceive disordered eating as a sign of weakness
- One in five people believe that people who binge eat ‘just lack willpower’
- One in four people believe eating disorders are choice and that people could stop if they really wanted to
- One in seven people believe that people with eating disorders ‘just want attention’
- One in four believe people with symptoms of eating disorders would only need to seek professional help if they became dangerously underweight.
Self-stigma can also be common among those with eating disorders. Stereotypes around what an eating disorder “should” look like leave many feeling as if they aren’t “sick enough” to be worthy of support. Eating disorders don’t discriminate and can impact anyone, of any age, weight, body size, gender, ethnicity, or sexuality.
“Eating disorders are scary and isolating, and nobody deserves to struggle on their own any longer than they already have. By identifying and supporting people that are at risk for, or showing early systems of body image concerns and/or disordered eating, we could prevent the development of an eating disorder, and change the course of someone’s life.” – Jemma (she/her), 24, QLD, member of Butterfly’s lived experience network, The Butterfly Collective
One third of people believe disordered eating behaviours are ‘pretty normal’.
But this is the greatest risk factor in developing an eating disorder – which has one of the highest mortality rates of any psychiatric illness.
A significant barrier to early intervention is that disordered eating and exercise behaviours and attitudes normalised and praised in society. This is often promoted by ‘diet culture’ – a set of ever-changing myths about food and bodies, promoting the idea that one’s body weight automatically equals health and that foods can be simplistically categorised as ‘good’ and ‘bad’.
Diet culture often encourages dieting and restrictive eating practices – which are forms of disordered eating. Disordered eating is one of the greatest risk factors in developing an eating disorder.
Knowing the signs and symptoms of disordered eating – and acting early – can help ensure an eating disorder doesn’t develop.
Lived experience insights
Get Involved in BIEDAW
There are many ways you can get involved with BIEDAW (5-11 September) to help spread awareness about eating disorders and body image, and encourage people to Know the Signs and Act Early.
Spread the message
Educate yourself about eating disorders
BIEDAW 2022 Events
BIEDAW is a collaboration between Butterfly, Eating Disorders Victoria, Eating Disorders Queensland, Eating Disorders Families Australia and ANZAED. Find out what events you can get involved with below.

Body Kind
Finding ways to like, accept, love or even feel positive about your body can be challenging in the world we live in today, but we can all try to be a little kinder.
Being Body Kind is how we nourish, nurture and move our bodies. It’s about the language we use out loud, online and in our heads – to ourselves and others.
This September, join Butterfly’s free annual awareness initiative, Body Kind, to encourage everyone in Australia to be kind to their own body and to others; face to face and online. You will receive practical, evidence-informed tips, activities and webinars.
BIEDAW on Socials
Keep your eyes on our social media channels, where across the week will be showcasing Lived Experience and expert insights, quotes and information on how you can reduce the impact of diet culture on your body image and life.
Instagram | Facebook | Twitter | LinkedIn
Donate
Donate to Butterfly, so we can continue supporting those living with eating disorders and body image concerns.
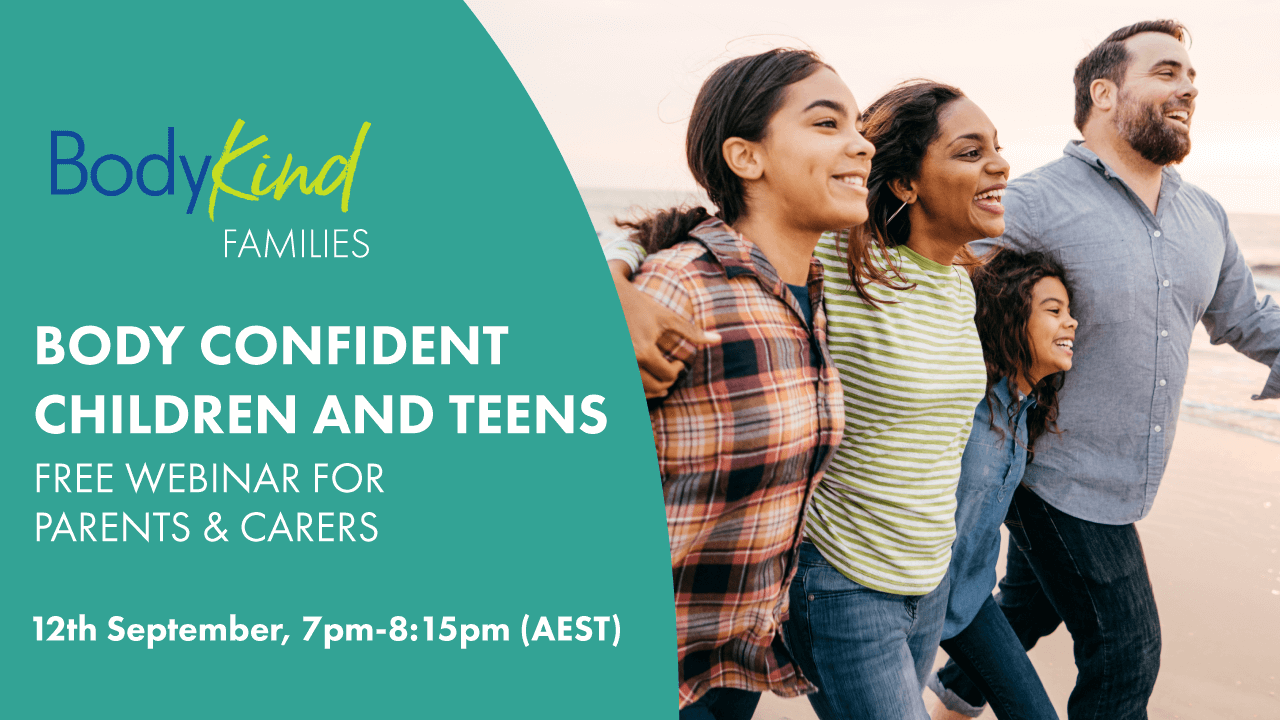
Free webinar for parents and carers
With a focus on prevention, this sessions provides information and practical tips to help parents better understand and promote positive body image in the home. Understand warning signs and the importance of early intervention, and what to do if you are concerned. Please note this is a live, online session and no recording will be available.
Mon 12th September, 7pm-8:15pm (AEST)
More about early intervention
- Eating disorders explained
- Body image explained
- NEDC: Early intervention
- Disordered eating and the diet cycle
Eating Disorder Alliance of Australia
- Butterfly Foundation
- Eating Disorders Victoria
- Eating Disorders Queensland
- Eating Disorders Families Australia
-
Australia and New Zealand Academy for Eating Disorders (ANZAED)

Concerned about yourself or someone you know? Get support now
If you or your loved one is experiencing a body image concern or eating disorder, contact the Butterfly National Helpline
1800 33 4673 | via webchat |email support@butterfly.org.au